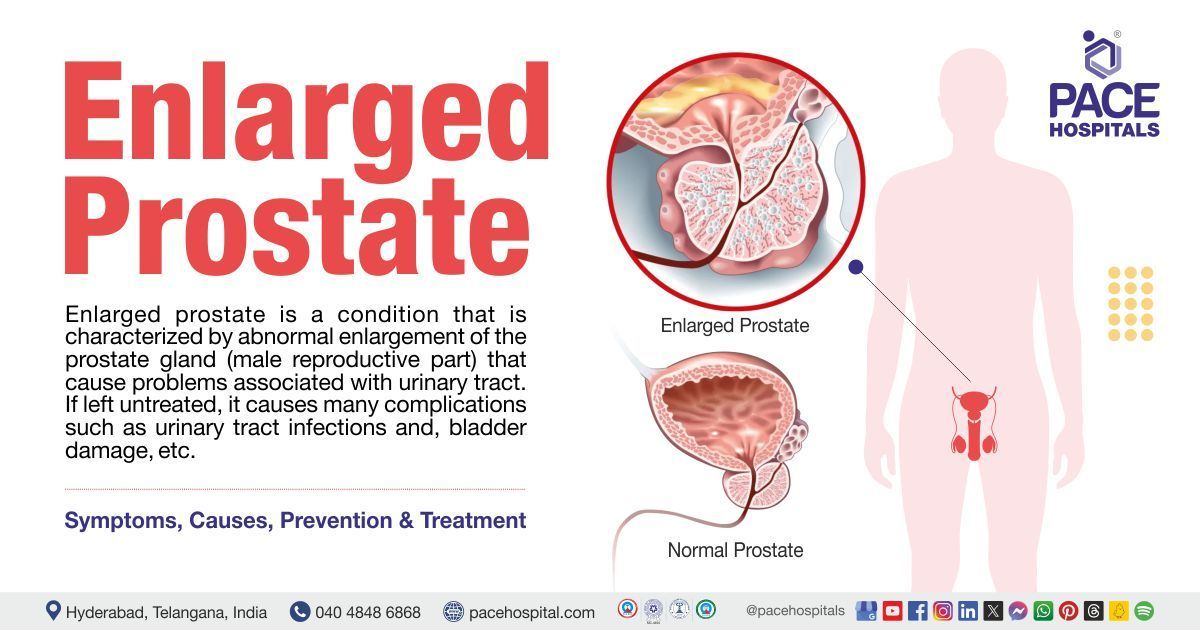
Urinary tract infection - Symptoms, Causes, Prevention and Treatment
Urinary tract infection definition
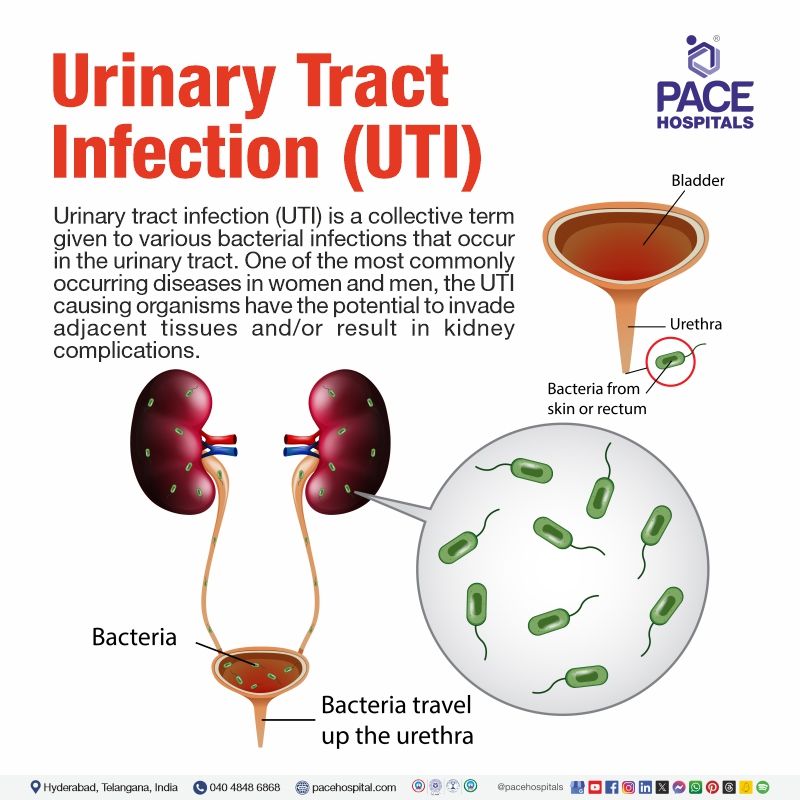
Urinary tract infection (occasionally called UTI infection) is a collective term given to various bacterial infections that occur in the urinary tract. One of the most commonly occurring diseases on the planet, the UTI causing organisms have the potential to invade adjacent tissues and/ or result in kidney complications. Nevertheless, with an appropriate antibiotic, UTI rapidly responds to antibiotic therapy prescribed by a urologist.
As such, the most common manifestation of UTI infection is acute cystitis (a type of bladder infection), which is far more prevalent among women than men; most clinical research on urinary tract infection has involved the women population. It has led to one of the common misconceptions that UTI infection is a gynaecological disease.
While it is true that UTI infection is overwhelmingly seen in women (approximately 1 in 3 females by 24 years), it is not a gynaecological disease, as this disease is also seen in men but less frequently.
Cystitis meaning
Cystitis is one of the common UTI infections. Cyst stands for "bladder-like bag or vesicle in an animal body", from the early Greek root “kystis," which meant "bladder, pouch", “-itis" is the word-forming suffix usually in medicine, which denotes "diseases characterized by inflammation" coming from the Modern Latin and Greek roots –“itis".
Prevalence of urinary tract infection worldwide
Mainly, the epidemiological properties that influence the type of urinary tract infection, causative agents, and resistance rates are age group, gender, geographical location, and setting. In the current era of high-resistance rates toward urinary tract infection antibiotics, the urologist may ask the history of the patient to understand the epidemiological information to understand which kind of pathogen could have caused the disease.
A diverse spectrum of pathogens, with a predominance of Gram-negative bacteria, is responsible for healthcare-associated urinary tract infections (HAUTIs). Pathogen spectrum can vary depending on healthcare setting, geographical locations, and clinical settings.
A European study demonstrated the increased prevalence of asymptomatic bacteriuria among diabetic women (26%) when compared with women without diabetes (6%).
Prevalence of urinary tract infection in India
A higher rate of E. coli followed by Klebsiella spp are the commonly seen pathogens across the globe. Comparatively, the studies from the Asian continent have reported reduced E. coli cases.
An Indian study from 2002 demonstrated the prevalence of E. coli as the most associated organism (64.3%), followed by Staphylococcus aureus and Klebsiella pneumoniae with (21.4%) and (14.3%) respectively. E. coli colonisation is higher in poorly controlled diabetics with HbA1C. An Indian study published in 2011 demonstrated that 42.8% of subjects from a sample of 1157 patients were suffering from UTI infection.
Types of urinary tract infection
Classification of urinary tract infection can be made according to the anatomical sites. Lower UTI infection could include diseases such as cystitis, urethritis, etc, while pyelonephritis can be included in upper UTI infection. It also differs from genders, such as bacterial prostatitis, epididymitis, orchitis, and epididymorchitis, which is seen in men. Delving deeper, the common types of UTI infections include:
- Uncomplicated cystitis: A bladder infection that occurs in an otherwise healthy, premenopausal, nonpregnant, female with a healthy urinary tract.
- Complicated cystitis: A serious bladder infection is usually caused by foreign body-induced cystitis (such as a catheter or stone), urinary tract abnormalities, instrumentation, or vesicoureteral reflux (urine moves backward - from the bladder to kidneys). Catheter associated urinary tract infection falls under this category.
- Uncomplicated pyelonephritis: Renal infection which occurs in an otherwise healthy, nonpregnant patient with a normal urinary tract.
- Recurrent UTI infection: Defined as ≥ 3 UTIs in 12 months or ≥ 2 UTIs in 6 months.
- Asymptomatic bacteriuria (colonization): If more than a lakh colony-forming units per milli litre (1,00,000 cfu/mL) of bacteria are seen in urine culture without any symptoms of illness or signs, it is called asymptomatic bacteriuria.
- Complicated pyelonephritis: A kidney infection during pregnancy or in a patient associated with other complicating factors, requiring hospitalisation.
- Interstitial cystitis: A condition of increased bladder pressure, pain and sometimes extending to the pelvis. It is also called bladder infection. It is also called honeymoon cystitis. If the infection lasts more than six weeks, it is called chronic cystitis.
UTI infection can also be stratified as healthcare-associated urinary tract infection (HAUTI) and community-associated urinary tract infection (CAUTI).
Urinary tract infection symptoms
Unfortunately, large numbers of patients with significant bacteriuria (bacteria in urine) are asymptomatic (doesn’t show symptoms). These patients may be normal, healthy patients, elderly patients, children, pregnant patients, and patients with indwelling catheters.
In the case of symptomatic cases, the common symptoms of UTI include:
- Pain in the abdomen, flank pelvic area, or lower back
- Pressure in the pelvic region
- Cloudy, foul-smelling urine
- Urinary incontinence (unintentional passing of urine)
- Frequent urination
- Urge incontinence (loss of bladder control leaning to inability to control urination)
- Painful micturition (also called dysuria - pain during urination)
- Hematuria (blood in urine)
- Fatigue (feeling extremely tired)
- Fever and chills
- Nausea and vomiting.
- Mental changes or confusion.
One of the most common male urinary tract infection symptoms is penis pain. Elderly patients frequently do not experience specific UTI infection symptoms, but they will present with
- Altered mental status
- Change in eating habits
- Gastrointestinal symptoms
In addition, patients with indwelling catheters or neurologic disorders commonly will not have lower tract symptoms, but flank pain and fever may be more pronounced.
Cystitis symptoms
The common cystitis symptoms include:
- Pain and burning or stinging type during urination
- Urine urgency
- Dark, cloudy or strong-smelling urine,
- Pain in the lower part of abdomen
Urinary tract infection causes
The most common cause of urinary tract infections (UTIs) is bacteria (most commonly Escherichia coli (E. coli)). These bacteria can enter the urethra (the tube that carries urine out of the body), and travel up the urinary tract, where they multiply and cause infection.
These are some other potential causes of urinary tract infections (UTIs):
- Sexual activity
- Incomplete bladder emptying
- Anatomical abnormalities (a shortened urethra or bladder prolapse)
- Medical conditions (Diabetes, kidney stones, usage of catheter)
- Weakened immune system
- Poor Hygiene or Improper Hygiene Practices
Urinary tract infection risk factors
The common risk factors that could enhance the risk and potentiality of urinary tract infection are as follows:
- Female gender
- Older age
- Urine incontinence
- Family history and genetics
- Catheterization
- Procedure
- Kidney or bladder stones
- Diabetes mellitus
- Immunocompromised status
- Female gender: In females, the anatomical distance from the urethral opening to the bladder is short when compared to that of males. It increases the chances of bacterial migration from the rectum to the urethral opening due to closer proximity, thus, enhancing the E. coli colonization and urinary tract infection progression.
- Older age: In the elderly (≥ 65 years, and particularly ≥ 80 years), the risk of male and female UTI infection is increased, and by 80 years of age, both genders have similar rates of UTI infection. Also, reduction in estrogen levels in postmenopausal women is another risk factor.
- Urine incontinence: This is one of the common risk factors which rapidly increases the risk of UTI infection by four times.
- Genetics and family history: A 2-4-fold increased risk of UTI infection is seen in the offspring (especially if it’s a girl) if the mother had UTI infections in her lifetime.
- Catheterization: Catheters are commonly used in hospitalized patients (accounting for about 70% of UTIs) which can significantly increase the urinary tract infection risk, especially with longer hospital stay. Catheterization issues such as neurogenic bladder, incomplete bladder emptying, etc all increase the risk of UTI infection, so as anatomic abnormalities of the genitourinary tract.
- Procedure: The risk of UTI infection increases during the immediate postprocedural days of any urinary tract procedure, such as flexible ureteroscopy indicated for stone management, etc. A Cochrane review demonstrated the beneficial aspect of urinary tract infection medication - antibiotic prophylaxis in patients assigned to procedures such as cystoscopy, reducing the risk of symptomatic UTI.
- Renal calculi or bladder stones: Stones display affinity towards bacteria, which can cause recurrent urinary tract infections. Ureteral stones associated with pyelonephritis can increase urosepsis risk.
- Diabetes mellitus: Sugar is a rich enabler of UTI infection, almost doubling it. When combined with obesity, the risk of urinary tract infection is even greater, but it is unclear if obesity is the cause.
- Immunocompromised status: In procedures such as renal or other solid organ transplant, the risk of urinary tract infection is increased. Nevertheless, human immunodeficiency virus (HIV) infection didn’t demonstrate any influence on the risk of bladder infection symptoms (symptomatic UTI infection), even in low CD4 count cases.
Pathophysiology of urinary tract infection
In general, there are usually three routes of urinary tract infection by which the organisms gain entry into the urinary tract:
- The ascending route,
- The hematogenous (descending), and
- Lymphatic pathways.
The female urethra is usually colonized by bacteria believed to originate from the faecal flora (bacteria seen in the stools). The short length of the female urethra and its proximity to the perirectal area enhance the pathogenesis of urinary tract infection by easing the colonization of the urethra. There are various other factors which enhance the colonization of the urethra.
- Modes of contraception: The use of spermicides and diaphragms as methods of contraception can serve as the basis of pathogenesis of urinary tract infection. Although there is evidence in females that bladder infections follow colonization of the urethra, the mode of ascent of the microorganisms is incompletely understood.
- Massaging and sexual intercourse: Massage of the female urethra and sexual intercourse allow bacteria to reach the bladder. Once bacteria have reached the bladder, the organisms quickly multiply and can ascend the ureters to the kidneys. This sequence of events is more likely to occur if vesicoureteral reflux (reflux of urine into the ureters and kidneys while voiding) is present. That UTIs are more common in females than in males because of the anatomic differences in location and length of the urethra tends to support the ascending route of infections as the primary acquisition route.
- Renal infection and hematogenous spread: Infection of the kidney by hematogenous spread (spread through blood) of microorganisms usually occurs as the result of dissemination of organisms from a distant primary infection in the body. Infections via the descending route are uncommon and involve a relatively small number of invasive pathogens. Bacteraemia (bacteria in blood) caused by S. aureus may produce renal abscesses. Additional organisms include Candida spp., Mycobacterium tuberculosis, Salmonella spp., and enterococci. Of particular interest, it is difficult to produce experimental pyelonephritis by intravenously administering common gram-negative organisms such as E. coli and P. aeruginosa. Overall, less than 5% of documented UTIs result from hematogenous spread of microorganisms.
- Renal lymphatic spread: There appears to be little evidence supporting a significant role for renal lymphatics in the pathogenesis of UTIs. There are lymphatic communications between the bowel and kidney, as well as between the bladder and kidney. There is no evidence, however, that microorganisms are transferred to the kidney via this route.
- After bacteria reach the urinary tract, three factors determine the development of infection: the size of the inoculum, the virulence of the microorganism, and the competency of the natural host defense mechanisms. Most UTIs reflect a failure in host defense mechanisms.
Complications of urinary tract infection
Given that urinary tract infection is a collective term for various types of diseases infecting the urinary tract, the complications usually vary. The maternal and fetal complications which arise from asymptomatic bacteriuria in pregnancy usually include the following:
Maternal complications
- Pre-eclampsia: Increased blood pressure during pregnancy
- Anaemia: Reduced red blood cells.
- Chorioamnionitis: Lower genitourinary tract infection migrating towards the amniotic cavity.
- Symptomatic acute cystitis: Bladder infection.
- Acute pyelonephritis: kidney inflammation
Foetal complications
- Intrauterine growth retardation: Foetus abnormal growth in the womb.
- Intrauterine death: Death of the foetus within the womb.
- Low birth weight: Less than 2500 g as per the World Health Organization (WHO)
- Prematurity: Baby born too early before the due date
Urinary tract infection prevention
There are various types of urinary tract infection prevention factors. These include:
- Hygiene practices
- Adequate fluid intake
- Urinate frequently
- Cranberry products and
- Probiotics
- Hygiene practices: Maintaining good hygiene, especially during using the toilet, can help in the prevention of the spread of bacteria from the anal area to the urethra.
- Adequate fluid intake: Drinking plenty of water to achieve enough hydration can help flush out bacteria from the urinary tract.
- Frequent urination: Regular emptying of the bladder can help in the prevention of bacteria buildup in the urinary tract.
- Cranberry products: Despite being ambiguous few studies suggest that cranberry products, (either its juice or supplements, may help in UTI infection prevention by inhibiting the bacterial adhesion to the urinary tract.
- Probiotics: Certain strains of probiotics, particularly lactobacilli, have shown promise in preventing recurrent urinary tract infections by restoring the natural microbial balance in the urogenital tract.
Screening for urinary tract infection
The definitive diagnosis is based on a positive urine culture, which is regarded as the gold standard. However, the process of obtaining clean-catch urine is cumbersome, and facilities for culturing urine might be lacking.
A urinary dipstick that incorporates leucocyte esterase (LE) and nitrite is an alternative screening tool for urinary tract infections and is especially useful in outpatients and at the bedside. A 2008 study from Ghana demonstrated that urine dipsticks that incorporate both nitrite and LE are slightly better than microscopy for pyuria as a screening test for urinary tract infection.
The screening test approach for urinary tract infection plays an important role in the healthcare system by supporting the clinicians in developing appropriate therapeutic decisions, monitoring not only renal and urinary tract diseases but also displaying an impactful aspect in on reducing the general healthcare cost and antimicrobial resistance.
Urinary tract infection diagnosis
The following are the usual diagnostic modalities:
- Blood test
- Urine Dipstick Test
- Urinalysis
- Urine Culture
Urinary tract infection treatment
The following are the usual treatment modalities:
- Fluid hydration
- Cranberry juice
- Lactobacillus probiotics
- Urinary analgesics
- Urinary tract infection antibiotics
FAQs - Frequently asked questions on Urinary tract infection (UTI)
-
How does a woman get a urinary tract infection?
Women get urinary tract infection if the microorganisms manage to enter the urinary tract through the urethra, infecting the bladder and eventually the kidneys in extreme cases. IT could be sexual intercourse, unhygienic fingers, or unhygienic restroom practices.
-
How to treat urinary tract infections naturally?
There are no natural remedies for urinary tract infection (cystitis treatment). The patient must consult the doctor so that prompt diagnosis can be made, after which appropriate and rational urinary tract infection antibiotics can be prescribed according to the sensitivity of the causative microorganism.
-
Is urinary tract infection dangerous?
No. Urinary tract infection is not a life threating disease, but it is recommended to obtain apt diagnosis with rational urinary tract infection treatment. In case of neglect, urinary tract infection could result in various symptoms and complications that can reduce patients' quality of life.
-
Can a urinary tract infection cause high blood sugar?
There hasn’t been any medical evidence to display the development of diabetes as a complication of urinary tract infection. On the contrary there is a huge chance of reverse case happenings. Diabetes with high blood sugar levels can increase the risk of developing urinary tract infections.
Is urinary tract infection contagious?
No, urinary tract infections are not typically contagious. Any disease can be termed contagious only if it is spread through touch (tactile contact). As such UTI infection is typically caused due to person's own gut flora, such as Escherichia coli, it cannot be termed as a contagious disease. Nevertheless, there are cases of urinary tract infection transmission through sexual intercourse. It is due to this reason that urination after sexual intimacy is recommended so as to flush out any microbes.
Does typhoid cause urinary tract infection?
Usually, no, but there have been rare cases of typhoid fever causing urinary tract infections. There have been reports of symptomatic urinary tract infections caused by Salmonella Typhi, the bacterium that causes typhoid fever. These urinary tract infections can occur in both immunocompromised individuals and immunocompetent individuals without any known urological abnormalities.
Do urinary tract infections go away?
No. Urinary tract infections do not go away without an antibiotic intervention. There are few cases in which healthcare specialists may prefer the "wait and watch" method (if the anomaly is found accidentally, the doctors see if it goes on its own before developing any complications). Urinary tract infections are not such case.
Why do I keep getting urinary tract infections?
People at times are contracted with recurrent urinary tract infection. While there could be various reasons, such as reinfection, usage of spermicidal products, anatomical abnormalities, hormonal changes and compromised immune system, the rise of antimicrobial resistance could pose as the most important factor.
What causes a urinary tract infection in a child?
Urinary tract infection in children is common with hygiene practices. While the majority (91-96%) of UTI infection in children is due to the bacterial ascent from the periurethral area to the urethra, it can be enhanced with hygiene sanitation practices.
Are bananas good for urinary tract infection?
While a direct connection to suggest that bananas specifically are good for urinary tract infections (UTIs) hasn’t been discovered, nevertheless, maintaining a healthy diet overall is important for supporting the immune system and overall health, which can help in the prevention of urinary tract infection.
Can sperm cause urinary tract infections?
No, sperm cannot cause urinary tract infections, but there are cases of UTI transmission through sexual intercourse. Staying well hydrated and maintaining hygiene during sanitation is one of the common way to prevent urinary tract infections. Also, urination after sexual intimacy can be done to flush out any microbes.
Can a urinary tract infection cause pain in testicles?
Yes, a urinary tract infection can cause pain in the testicles. Urinary tract infections can sometimes spread to the epididymis (a structure located behind the testicles). This condition, known as epididymitis, can cause pain, swelling, and tenderness in the testicles.
Can a urinary tract infection cause erectile dysfunction?
While there hasn’t been any direct evidence suggestive of a urinary tract infection causing erectile dysfunction, it must be understood that consecutive appearances of both in a patient could suggest an underlying disorder related to overall health and well-being.
Usually, long-term diabetes can contribute to both urinary tract infections and erectile dysfunction.
Which doctor treats urinary tract infection (UTI)?
The type of doctor you see for a urinary tract infection (UTI) depends on several factors, including your gender, age, severity of symptoms, and any underlying medical conditions, such as:
- General Physician: Most uncomplicated UTIs in women and men with no underlying conditions can be diagnosed and treated effectively by a General Physician. They can perform a urine test, prescribe antibiotics, and offer advice on preventing future infections.
- Urologist: In case of recurrent UTIs, complex UTIs involving the upper urinary tract (kidneys, ureters), or underlying conditions like kidney stones or bladder blockage, a urologist might be the best choice. They have expertise in diagnosing and treating complex urinary tract issues.
- Gynecologist: While urologists are more specialized in the urinary tract overall, gynecologists are familiar with UTIs in women and can often diagnose and treat them effectively. They may also consider potential female-specific, especially those with concurrent vaginal infections, pregnancy or concerns about sexual health.
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.

Our Locations
Subscribe to our newsletter and stay updated with the latest health information.
By clicking on subscribe now, you accept to receive communications from PACE Hospitals on email, SMS and Whatsapp.
Subscribe to PACE Hospitals News
Thank you for subscribing. Stay updated with the latest health information.
Oops, there was an error. Please try again submitting your details.
-

Payment in advance for treatment (Pay in Indian Rupees)
For Bank Transfer:-
Bank Name: HDFC
Company Name: Pace Hospitals
A/c No.50200028705218
IFSC Code: HDFC0000545
Bank Name: STATE BANK OF INDIA
Company Name: Pace Hospitals
A/c No.62206858997
IFSC Code: SBIN0020299
Scan QR Code by Any Payment App (GPay, Paytm, Phonepe, BHIM, Bank Apps, Amazon, Airtel, Truecaller, Idea, Whatsapp etc)
Call us at 04048486868
ADDRESS
PACE Hospitals
Hitech City : Beside Avasa Hotel, Pillar No. 18, Hyderabad - 500081
Madinaguda: Mythri Nagar, Beside South India Shopping, Madinaguda, Hyderabad - 500050
QUICK LINKS
Disclaimer
General information on healthcare issues is made available by PACE Hospitals through this website (www.pacehospital.com), as well as its other websites and branded social media pages. The text, videos, illustrations, photographs, quoted information, and other materials found on these websites (here by collectively referred to as "Content") are offered for informational purposes only and is neither exhaustive nor complete. Prior to forming a decision in regard to your health, consult your doctor or any another healthcare professional. PACE Hospitals does not have an obligation to update or modify the "Content" or to explain or resolve any inconsistencies therein.
The "Content" from the website of PACE Hospitals or from its branded social media pages might include any adult explicit "Content" which is deemed exclusively medical or health-related and not otherwise. Publishing material or making references to specific sources, such as to any particular therapies, goods, drugs, practises, doctors, nurses, other healthcare professionals, diagnoses or procedures is done purely for informational purposes and does not reflect any endorsement by PACE Hospitals as such.